Contact Us
Latest News
- Clues beginning to emerge on asymtomatic SARS-CoV-2 infection
- Back in November of 2020, during the first wave of the COVID-19 pandemic, I was teaching an in-person microbiology laboratory. One of my students had just been home to see his parents, and they all c…
- Read more
- Could there maybe be better uses of genetics and probiotics?
- Professor Meng Dong and his laboratory have created a probiotic that can metabolize alcohol quickly and maybe prevent some of the adverse effects of alcohol consumption. The scientists cloned a highl…
- Read more
- ChatGPT is not the end of essays in education
- The takeover of AI is upon us! AI can now take all our jobs, is the click-bait premise you hear from the news. While I cannot predict the future, I am dubious that AI will play such a dubious role in…
- Read more
- Fighting infections with infections
- Multi-drug-resistant bacterial infections are becoming more of an issue, with 1.2 million people dying of previously treatable bacterial infections. Scientists are frantically searching for new metho…
- Read more
- A tale of two colleges
- COVID-19 at the University of Wisconsin this fall has been pretty much a non-issue. While we are wearing masks, full in-person teaching is happening on campus. Bars, restaurants, and all other busine…
- Read more
( 39835 Reads)
None Max
Learning Objectives
- Define the primary tissues of the immune system.
- Define the secondary tissues of the immune system and their function.
- Explain the function of the circulatory and lymphatic system in the immune system.
- Understand the role of the bone marrow in the immune system.
- Describe the role of phagocytes, polymorphonuclear cells, mast cells, monocytes, macrophages, and lymphocytes, in the immune system.
- Describe the function and structure of the lymph nodes, MALT and the spleen.
The Immune System Is a Complex Collection of Organs, Tissues, and Cells
The immune system consists of a complex network of organs and tissues, connected by blood and lymphatic vessels, that work together to prevent infection. Many of these systems are unleashed by activation of other parts of the immune system. The extensive interdependence of the players of the immune system can make it difficult for the beginning student to understand. As we go through the immune system, you will encounter unfamiliar terms, but be patient because they will be explained later in the chapter. To try to make it a bit easier, we will first describe the anatomy of the immune system, then examine the various cell types involved in immunity, and finish by describing how these parts work together in reacting to an invading pathogen.
Many different organs and tissues in the body contribute to the function of the immune system. These include the circulatory system, bone marrow, thymus, spleen, lymphatic system and Mucosal Associated Lymphoid Tissue (MALT). Together these tissues are responsible for the creation, transport and successful operation of mammalian immunity. In this section we will look at the role of each tissue and introduce a number of cells and proteins involved in immunity.
The tissues of the immune system fall into two groups based upon their role in host defense. Primary (or central) tissues look after immune cells, creating and educating them during their differentiation into mature cells. The bone marrow and thymus gland are parts of the primary immune system. Secondary (peripheral) immune organs look after mature cells that are an active part of defense. The secondary system encompasses the rest of the immune tissues: the spleen, the lymphatic system, lymph nodes and MALT. Of course it is not this simple and the spleen and MALT also help in the maturation of immune cells. Figure 15.2 shows the anatomy of the blood and lymph systems.
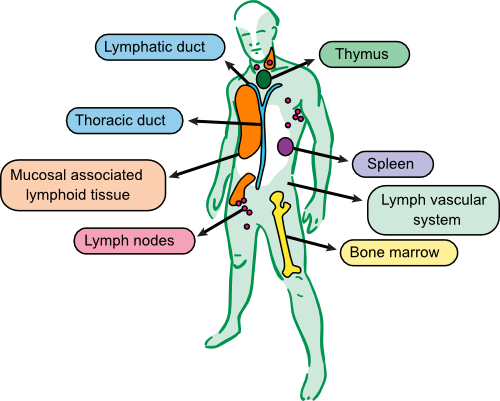
Figure 15.2. The tissues of the immune system. A large collection of organs and tissues are involved in the immune system of animals. Some of these tissues create and or educate the immune system, bone marrow and thymus, while other parts are involved in fighting infections, lymph systems, lymph nodes, spleen and MALT. The thoractic duct collects liquid from the lymph system and returns it to the circulatory system at the left subclavian vein near the heart.
The Circulatory System Transports the Components of the Immune System
The circulatory system is responsible for the transport of blood throughout the body and consists of the heart, the lungs and the vascular system of arteries, capillaries and veins. Blood, which runs through this vascular system, contains both cellular and non-cellular components. The major cell type found in blood are red blood cells, whose role is to transport oxygen and carbon dioxide into and out of the body respectively. The circulatory system also plays a secondary role as one of the routes immune cells use for transport around the body. Blood contains many types of what are called white blood cells, which are made up of mainly neutrophils, but also monocytes, T-lymphocytes and B-lymphocytes.
The non-cellular portion of the blood is a liquid called plasma. A major constituent of plasma is immunoglobulins (antibodies). It also contains various proteins of the complement system, which are equally important in the immune system. Plasma also contains the protein fibrinogen as a major component. Under the right conditions, fibrinogen participates in a complex series of reactions that eventually result in the formation of a fibrin clot in the blood. Platelets also participate in this process. Blood clots are important in stopping bleeding and also in inhibiting the invasion of advancing pathogens by entrapping them.
Bone Marrow Is the Origin of All Immune Cells
The bone marrow is the source of many immune and blood cells in the healthy adult animal. If the bone is split lengthwise, a marked difference in tissue is noticed. Part of the tissue is red, which is the source of red and white blood cells. The other portion is yellow adipose tissue that is inactive. During an infection, the yellow marrow can be reactivated to become red marrow to help in the production of larger numbers of immune cells.
In the adult animal, all immune cells originate from hematopoietic stem cells located in the bone marrow. Stems cells constantly divide and differentiate into various types of immune cells under the influence of cytokines (cytokines are small signaling proteins that help to regulate the behavior of the cells of the body). Figure 15.3 shows the origin of the cells of the immune system. The bone marrow is ultimately responsible for the synthesis of eight types of cells: red blood cells, platelets (through megakaryocytes), neutrophils, basophils, eosinophils, mast cells, monocytes/macrophages, T lymphocytes (T cells) and B lymphocytes. Some of these cell types mature in the bone marrow itself, while others migrate through the circulatory system and undergo final maturation in other tissues. At this point, we will take a short stop and look briefly at some of the features of the cells created in the bone marrow as an introduction to their function. You will learn more details about each immune cell type later when we cover specific immune responses.
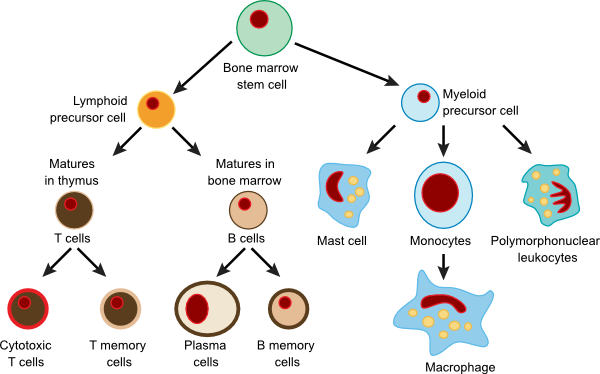
Figure 15.3. Types of immune cells and their progenitors. In humans stem cells differentiate into different types of immune cellsin the bone marrow under the influence of different cytokines.
Stem Cell Research
Stem cells are of great interest to physicians, researchers and the public due to their potential benefit in a number of important human diseases. There is great confusion as to what a stem cell is, where they come from and their function. So before we go on, let's try to clear up some of that confusion. Embryonic stem cells are completely undifferentiated cells that are found in the developing embryo and can potentially mature into any kind of tissue. These types of cells are most often associated with a developing fetus and are not found in adults. Adult stem cells, of which hematopoietic stem cells are one class, are undifferentiated cells found among differentiated cells in a tissue or organ. They can renew themselves and develop into the specialized cell types of that organ. Adult stem cells have been found in many tissues, including the bone marrow, the brain, the digestive tract, and the skin.
James Thompson of the University of Wisconsin-Madison was the first to obtain embryonic stem cells by taking them from a growing embryo. These cells are the progenitors of all the cells in the body and are unique in a number of ways.
- Embryonic stem cells can proliferate indefinitely. Typical mammalian cells are capable of a limited number of divisions. After about 20-50 cell cycles, they are incapable of dividing further. This occurs because at each division a small portion of the ends of the chromosomes, called telomeres, is lost. Initially, this is acceptable because the telomere does not contain vital DNA. However, as subsequent divisions proceed, the cells lose more and more of the telomeres and eventually the chromosomes fail to function. Embryonic stem cells get around this difficulty by activating an enzyme called telomerase. Telomerase adds extra DNA onto the ends of chromosomes during division so that they do not shorten.
- Because of the role of embryonic stem cells in normal development, they have the capability of differentiating into any cell type. In contrast, mature differentiated cells have their function dictated by a fixed pattern of gene expression. We currently do not know how to revert differentiated cells to a more undifferentiated state. As a consequence stem cells offer the best hope for generating useful cell types for various treatments.
Research on embryonic stem cells may result in a number of promising developments. Having these cells available for research will give us new insight into how humans and other mammals develop. It seems clear that embryonic stem cells develop into other cells types and tissues under the influence of cytokines. By studying the process we will learn what these signals are and how they work. Being able to create an unlimited supply of different cell types may eventually allow the development of new tissues and organs for use in transplants. Presently, there is a great need for organs and tissues for ailing patients. Scientists have already been able to create lungs, bladders and kidneys in animal experiments. These cells may also lead to the creation of cures for brain disorders such as Alzheimer's and Parkinson's diseases.
Embryonic stem cells are also controversial because to obtain them, it has been necessary to destroy a developing embryo. A fertilized egg is allowed to divide for a period of time and then the cells are extracted. Some consider this equivalent to killing a human being, but the key to the controversy is when we decide a human life begins. Does it begin the minute that a mass of cells has the potential to develop into a human? Does it begin when that group of cells can survive on its own? Medicine is getting better at saving babies born prematurely. What if a time comes when an embryo can be raised completely out of the uterus? Scientists cannot and should not make these decisions by themselves. Human society must decide what is acceptable and the key to making good decisions is educating ourselves about the issues.
Research in the years since Dr. Thompson's first efforts has begun to demonstrate that adult stem cells may be able to replace embryonic stem cells for some purposes. But at the present time, undifferentiated, embryonic stem cells are still necessary for many important experiments.
Cells Made in the Bone Marrow
Hematopoietic stems cells create a large number of red blood cells. The heathy human creates 2.4 million red blood cells per second and they are essential for moving oxygen in and carbon dioxide out of our system. Another cell type produced in the bone marrow are megakaryocytes. These then differentiate into platelets that are necessary for the formation of blood clots following any kind of injury. Blood clots are vital in stopping the flow of blood when blood vessels are injured, but also have a role in fighting infections (see below).
Polymorphonuclear granulocytes is the general term given to neutrophils, eosinophils and basophils. The first half of the name describes the appearance of the nucleus that seems to be split into a number of different lobes. In reality, the nucleus is contiguous, but contains many infoldings, which give it a polynuclear appearance. The rest of the name comes from the appearance of the cytoplasm, which looks speckled. The cytoplasm is full of granules that contain compounds and enzymes important in fulfilling the function of each cell type. Polymorphonuclear granulocytes make up 50-70% of the white blood cells found in blood. They last only about three days and have to be replaced at a rate of 80 million cells per minute.
Neutrophils are the most common type of polymorphonuclear cells, making up 90% of granulocytes in the blood. These cells function as phagocytes in attacking and destroying infectious agents. We will cover their roles in more detail when we discuss phagocytes.
Eosinophils make up 2-5% of granulocytes in the blood, but this number can rise considerably in people with parasitic diseases as well as asthma, eczema or other diseases associated with allergies. They are primarily found in the blood, but also near epithelia that have high bacterial populations (e.g., intestines, vagina, nasal passages). The granules in these cells bind the red dye eosin, giving the cells their name. Eosinophil granules contain a number of different enzymes including, acid phosphatase, glucuronidase, cathepsins, RNase, and arylsulfatase and peroxidase. They also produce toxic basic proteins. They respond to the chemical signals put out by other immune cells and can then participate in an immune response. The major reactions take three forms.
- They can down-regulate an immune response by destroying histamine secreted by mast cells using the enzyme histinase. Eosinophils also liberate arylsulphatase that breaks down the slow reactive substance of anaphylaxis (a dangerous form of allergic response) that is released by mast cells.
- Eosinophils combat antigenic challenges too big to be attacked by phagocytes. Examples of such challenges are parasitic worms or helminths. In battling these infections, the body first covers the worm with antibody. This then activates eosinophils, which bind to the parasite and release the contents of their granules, thus causing external digestion of the worm.
- As is the case with neutrophils, eosinophils can phagocytize microorganisms, but this is a secondary role.
Basophils are small cells that make up less than 1% of all white blood cells. The granules of these cells contain heparin, histamine, decarboxylase, histidine, dehydrogenase and diaphorase. Heparin is an important anti-clotting compound, and histamine finds its use modulating the immune response. Histidine is converted to histamine by decarboxylase. The role of basophils in the immune response is not yet clear, but they seem to play a role in the defense against parasitic worms and in severe allergic reactions. They have a very high affinity for one class of antibodies (IgE) and they are usually found coated with IgE in tissues. Binding of IgE may set in motion a series of events that causes other immune cells to respond to the high concentrations of IgE. Basophils may be cellular alarms that notify the rest of the immune system and help to concentrate the point of attack.
Mast cells are closely related to basophils but are distinct in their reactions to antigens. They are found throughout the body in lymph nodes, spleen, bone marrow, around blood vessels, nerves, glands and in the skin. Mast cells have granules that, like basophils, contain heparin and histamine. They have a high affinity for IgE as well and their activation by antigen triggers histamine release. Until recently, they were mostly thought to trigger unwanted allergic reactions, but it is now becoming clear they participate in immune responses to Gram-negative bacteria and to nematodes, such as the hookworm. Their wide distribution indicates that they are important in many immune responses.
Monocytes and macrophages are long-lived specialized phagocytic cells. Monocytes are migrating phagocytic cells found in the bloodstream and when they enter other tissues, they differentiate into macrophages. Macrophages are found in the brain, lungs, liver, spleen, lymph nodes, joints and peritoneum. The key functions of monocytes and macrophages are to remove our own dead cells when they reach the end of their useful life and also to remove pathogens. For example macrophages in the liver, called Kupffer cells, phagocytize old erythrocytes from the blood and remove them. Another one of their functions is the creation of important immune proteins and peptides. They are responsible for synthesizing transferrin (an iron-binding protein), and various cytokines necessary for immune function. Macrophages also synthesize some of the complement proteins.
B lymphocytes or B cells can differentiate into plasma that are responsible for antibody production. They are very important in fighting many different types of infections, especially, bacterial infections. T lymphocytes are involved in regulating the immune system and destroying host cells that are out of control, either due to a breakdown in cell division regulation (cancer) or infection by a virus or even an intracellular parasite. We will discuss the functions of these cells in more detail when we cover the adaptive host response.
The thymus is a fist-sized organ located above the heart that is involved in the maturation of T lymphocytes (also referred to as T cells). T cells produced by the bone marrow are immature and journey to the thymus through the bloodstream. The blood vessels that supply the thymus with oxygen and other nutrients also contain a blood-thymus barrier that only allows immature T cells in and mature T cells out. The thymus is also connected to the lymphatic system through lymph vessels. We will talk more about thymus function when examining T cell maturation later in the chapter.
The Lymphatic System Is a Separate Vascular System Through Which Lymph and Immune Cells Move
The lymphatic system is a separate vascular system, distinct from the bloodstream, through which the lymph moves. It is a branching system whose vessels get ever smaller as it penetrates tissue. Unlike the blood system, the lymphatic system is not circular, instead its capillaries extend into tissues and eventually having closed ends. The system focuses its attention on areas of the body that are most likely to be entry points for pathogens: skin dermis, respiratory tract, gastrointestinal tract and genitourinary tract. It functions are:
- To collect excess fluid from surrounding tissue and return it to the bloodstream
- To absorb fat from the villi of the small intestine.
- For the transport of Immune cells moving through the body
Here we will focus on its major roles of the lymph system, harboring and transporting many of the cells involved in the immune system. Lymph fluid consists of leukocytes and many components of plasma, but does not contain red blood cells. Liquid enters the lymph system from non-vascular tissue draining into lymph capillaries. The capillaries then drain into lymph nodes that sit at the junction of a number of lymph vessels.
Lymph nodes, shown in Figure 15.4, are found throughout the body and are major centers for immune function. In a healthy adult the smallest lymph nodes are a few millimeters in diameter, while the largest can reach 2 cm. Large volumes of liquid and cells pass through lymph nodes each day and are filtered to detect antigens and remove microbes. The nodes also interact with phagocytes to begin various immune functions that we will elucidate later. Lymph nodes are dynamic, densely packed structures with the bulk of the cells inside them being mobile. Phagocytes and antigens enter through as many as five vessels, called afferent ducts. The lymph node contains large numbers of B- and T-lymphocytes, but macrophages and plasma cells are also present. Macrophages carry out the job of filtering the incoming fluid and plasma cells (effector cells that differentiate from antigen-stimulated B cells) secrete antibodies that exit along with other immune cells by the single exit, the efferent duct. The lymphatic system then merges into larger vessels and eventually reconnects to the circulatory system through ducts near the heart. The flow of liquid is therefore from the lymphoid capillaries, into lymph vessels and eventually exiting into the bloodstream at the heart. There are actually two asymmetric lymphatic drainage systems, the both drain into veins near the heart. The right lymphatic duct drains the upper right side of the body, including the right side of the head, the heart and lungs, into the right subclavian vein. The rest of the body drains into the thoracic duct, which then drains into the left subclavian vein. Liquid entering the lymphatic system from the blood and extravascular tissue filters through typically eight to ten nodes before returning to the bloodstream.
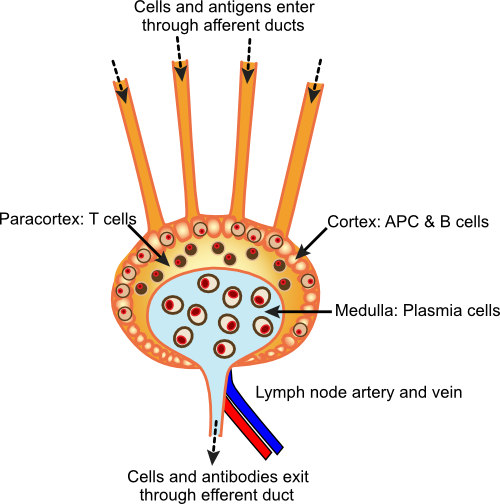
Figure 15.4. A diagram of a lymph node. Lymph nodes contain many types of immune cells organized to monitor and react to antigens that come in from the lymph system. T cells and B cells line the edges of the lymph node and plasma cells and phagocytes are found in the core.
The MALT and Spleen Are Collections of Immune Cells That Work to Fight Infection
Mucosal-Associated Lymphoid Tissue (MALT) is scattered throughout the connective tissues of the body, but especially beneath moist epithelial membranes such as those that line the upper respiratory tract, intestine and urinary tract. MALT is strategically distributed to help the body prevent infection by organisms that have penetrated beyond the mucosal surface. MALT consists of small masses of lymphatic tissue (up to a millimeter in diameter) containing mainly lymphocytes. These tissues are far less organized than the lymph nodes. Most MALT consists of small groups of cells, but in certain areas it is found in large clusters. For example, large aggregates of MALT occur in the wall of the lower portion (ileum) of the small intestine and are known as Peyer's patches. Tonsils and adenoids are also aggregates of MALT that protect your body from microorganisms present in the upper respiratory tract.
The spleen is a very important secondary lymphoid organ. Individuals who have had their spleens removed due to rupture caused by a car accident or atrophy from sickle cell anemia can lead nearly normal lives, but they tend to be more susceptible to infection. Some functions of the spleen are similar to those of the lymph nodes; however, it also produces lymphocytes and removes senescent (old) red blood cells from the circulation.
The spleen, shown in Figure 15.5, is highly organized and is a repository for immune cells. It plays an important role in response to pathogens. The spleen contains a circulatory system allowing access to it through the blood. Cells in the spleen organize around the blood vessels into two tissues: red pulp and white pulp. Red pulp contains mainly red blood cells, and white pulp is made up predominantly of lymphocytes. The white pulp focuses tightly around the arterioles of the spleen while the red pulp fills the rest of the interstitial space. The location of various lymphocytes in the white pulp further differentiates it. T cells are found near the arterioles and further away are areas of B cells. The spleen is a major area for B cells to congregate in the body, where they wait to be activated by antigens. During an illness, activated lymphocytes are released from the spleen to fight the infection.
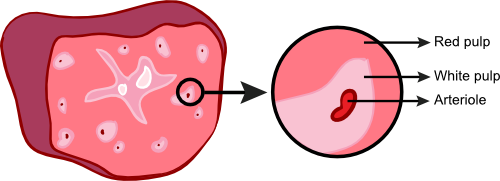
Figure 15.5. Anatomy of the spleen. The spleen is located on the middle of the abdomen to the left of the stomach. This cartoon of a cross section of the spleen shows both red and white pulp. The magnified section shows the arrangement of cells. The white pulp near the arterioles consists of T cells and B cells and the red pulp is filled with red blood cells.
This completes our tour of the anatomy of the immune system. In the next section we will more specifically examine how cells and compounds in these tissues recognize and attack invading pathogens.
Key Takeaways
- Many different tissues distributed throughout the body are involved in protecting us against microorganisms. The immune system can be divided into primary (or central) tissues: the bone marrow and thymus, and secondary (or peripheral) tissues; the spleen, the lymphatic system, lymph nodes and MALT.
- Primary tissues create and educate immune cells, while secondary tissues monitor the body for invading pathogens.
- The bone marrow creates phagocytes (neutrophils, basophils, monocytes and macrophages), mast cells and lymphocytes, all of which are important in the immune response.
- Phagocytes ingest and kill cells identified for destruction by the immune system.
- Mast cells are present in many immune tissues and react to incoming antigens, alerting the rest of the immune system.
- Lymphocytes are divided into two forms, T cell and B cells.
- Lymph nodes and the lymph system are a secondary vascular system that monitors the body for antigens. The lymph node contains T cells, B cells and macrophages.
- The spleen is also a reservoir of B cells, T cells that are released when activated to fight an infection.
Quickcheck 15-4
Warning, you must be logged in to be able to have your exam graded. Answer the questions below and if you are a registered user of the site you will see a Grade Exam button. Click it to have your exam graded.